Luis Leone
We call cardiomyopathies the involvement of the cardiac muscle fibers. The affectations of the cardiac muscle can correspond to multiple etiologies, known and unknown.
Causes of cardiomyopathies and / or myocarditis: (World Health Organization Classification)
|
Inflammatory
Metabolicas
|
necrolysis
Infiltrative
|
Hematologic
Hypersensitivity
Genetics
Neuromuscular
Postpartum
|
Forms of presentation: within cardiomyopathies there are three forms:
A) Dilated B) Hypertrophic C) Restrictive.
These three forms are characterized by presenting different histopathological and morphological characteristics and determining different clinical pictures.
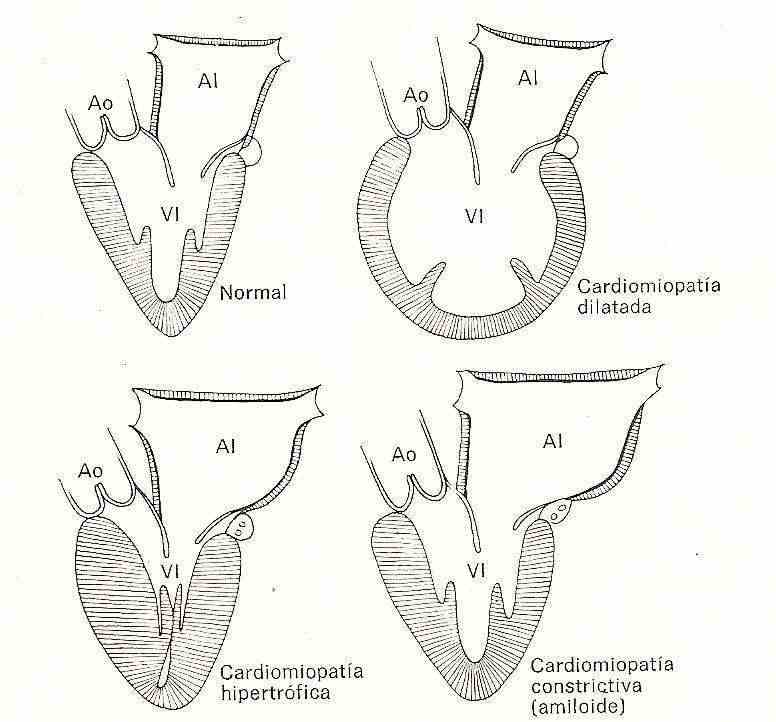
A) Dilated
As its name indicates, it is characterized by the microscopic predominance of marked dilation of the cardiac cavities, with increased weight of the heart, thickened walls but predominant dilation of the atria and ventricles, valve rings, presence of clots and thrombi, areas of extensive fibrosis over the ventricles, endocardial thickening with marked areas of disruption that are located in both the left and right ventricles.
Microscopically, extensive areas of interstitial and perivascular fibrosis are observed, with areas of necrosis, inflammatory cell infiltrate, hypertrophy of myocytes, degeneration of muscle fibers with an increase in the size of myofibrils, an increase in the number of mitochondria and sarcomeros, alterations of the nuclei, presence of lipid vacuoles and loss of myofilaments. These alterations are related to the etiological causes and their variations may be to a greater or lesser degree. In acute phase chagas, the presence of parasites can be observed in the cardiac fibers.
Symptoms : heart failure syndrome, presence of pulmonary or systemic embolisms.
Physical examination : gallop rhythm with R3 and R4, bilateral edema, presence of ascites, hepatosplenomegaly, bilateral rales.
The toe shock is displaced to the left, it may not be palpable due to the presence of pericardial effusion, accompanied by significant jugular engorgement without collapse, a paradoxical peripheral arterial pulse, and a drop in blood pressure on inspiration.
Radiology : cardiomegaly, pleural effusions, venocapillary hypertension, flow redistribution.
ECG : sinus tachycardia, presence of atrial or ventricular arrhythmias, ST segment and T wave abnormalities, presence of different degrees of conduction disorders.
Echocardiogram : marked dilation of the ventricular and atrial cavities, global hypokinesia, areas of dyskinesia, presence of pericardial effusion, decrease in the shortening fraction.
Gamma camera studies Radiocardiogram : marked decrease in ejection fraction.
Angiography : severe dilation of the left and right ventricular cavity, global hypokinesia, secondary mitral and tricuspid regurgitation due to dilation of the annulus, elevation of left ventricular end-diastolic pressure and pulmonary pressure, decreased minute volume.
Among the etiological causes, we must point out that on many occasions the damages produced can be partially or totally reversible, keeping a direct relationship with early diagnosis and correct treatment; examples of this are the toxic effects of chemotherapy drugs, alcohol and the correct treatment of bacterial and viral causes.
Arrhythmogenic dysplasia is the only one with direct involvement of the right ventricle in the outflow tract, with partial or total replacement of muscle tissue by adipose tissue and fibrosis, which facilitate the reentry mechanism for the generation of severe ventricular arrhythmias, which is why which these patients have a high risk of sudden death.
The treatment of this heart disease does not differ from the treatment for heart failure, and is mainly based on: beta blockers, diuretics, antialdosteronics, and renin angiotensin system inhibitors. The development of rhythmic events sometimes requires the use of antiarrhythmic drugs such as amiodarone, and in many of these patients anticoagulation is indicated, due to their dilated chambers, low ejection fraction, and the increased risk of presenting embolic events.
The development of a higher degree of cardiac dilation results in heart failure and a severe increase in mortality, which in these patients is approximately 50% at 5 years after diagnosis, presenting not only due to hemodynamic deterioration, It also adds the risk of sudden death that is very high in this population, which is why the implantation of a cardioverter-defibrillator and / or ventricular resynchronization plus cardioverter-defibrillator is added for the treatment of these patients.
Hypertrophic cardiomyopathy
The pathological alterations are characterized by a marked increase in ventricular mass with reduction of the ventricular cavities, it presents with a greater degree in the left ventricle and lower degrees of associated hypertrophy of the right ventricle are observed. Generally there is dilation of the atrial cavities, with reduction of the ventricles as a consequence of the increased thickness of the walls.
Hypertrophy can be symmetric or asymmetric, in the latter the increase in thickness predominates
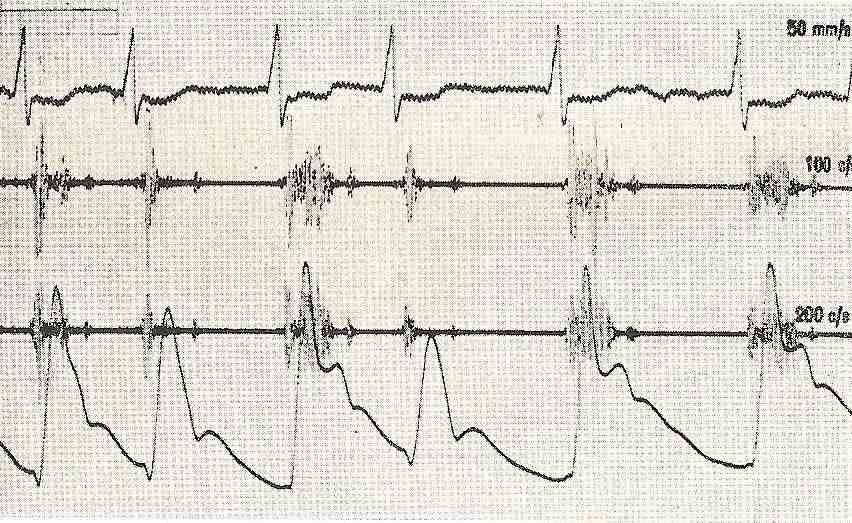 Figure 2 Hypertrophic cardiomyopathy, ejection systolic murmur, finger-like pulse, note the second notch in the descending branch of the pulse, carotid in complex 3 and 5, before the dicrotic incisuration of the interventricular septum and as a consequence, obstruction in the tract outflow of the left ventricle, determined by the hypertrophic interventricular septum and the anterior leaflet of the mitral valve, which during ventricular systole undergoes a “venturi” effect of absorption against the interventricular septum, determining the reduction in the volume of expulsion. The concentric variety does not exist obstruction, but determines a reduction in the filling of the ventricle with the corresponding increase in intraventricular pressure, caused by the lack of compliance of the walls (decrease in ventricular compliance).
Figure 2 Hypertrophic cardiomyopathy, ejection systolic murmur, finger-like pulse, note the second notch in the descending branch of the pulse, carotid in complex 3 and 5, before the dicrotic incisuration of the interventricular septum and as a consequence, obstruction in the tract outflow of the left ventricle, determined by the hypertrophic interventricular septum and the anterior leaflet of the mitral valve, which during ventricular systole undergoes a “venturi” effect of absorption against the interventricular septum, determining the reduction in the volume of expulsion. The concentric variety does not exist obstruction, but determines a reduction in the filling of the ventricle with the corresponding increase in intraventricular pressure, caused by the lack of compliance of the walls (decrease in ventricular compliance).
Macroscopically, an increase in cardiac mass is observed, and hypertrophy can be located in different positions, with the apical and midseptal patent being two recognized variants, the latter prevailing in Japan.
Histologically, hypertrophy with great disorganization of the muscle cell bundles, myofibrillar disorganization, interstitial fibrosis, and alteration of the cell nuclei are recognized.
Symptoms : dyspnea, chest pain, syncope and palpitations.
Physical examination : ejection systolic murmur of intensity 3 to 4/6 mid-systolic with irradiation to foci of the base and murmur of mitral regurgitation in mitral area of intensity 2/6 protomesositolico. Sometimes this may not be manifest or be masked by the ejection murmur. The characteristic of this ejection murmur is determined by its increase with the Valsalva maneuver, during the compression phase. When this maneuver occurs, there is a decrease in venous return to the right chambers, pulmonary circuit and as a consequence a decrease in the filling of the left ventricle that increases the obstruction of the tract, determining a frank increase in the murmur.
In the examination of the patient with the obstructive variant, we can find the palpation of the arterial pulse as a second lower intensity projection determined by the dynamic obstruction during the expulsive phase, called the finger pulse.
The tip shock is preserved, manifesting energetic and sustained.
Radiology : a moderate increase in the size of the cardiac silhouette is observed, with an increase in the left atrium and signs suggestive of left ventricular hypertrophy.
ECG : signs of left atrial growth and left ventricular overload, Q waves may also be present in precordial, suggesting septal hypertrophy.
Atrial and ventricular arrhythmias are frequent, and the presence of atrial fibrillation is a worrying incidence, which can motivate its hemodynamic decompensation, by reducing the filling of the left ventricle.
Echocardiogram : it is the method that allows immediate diagnosis by allowing us to observe the increase in the left atrium, hypertrophy of the septum or ventricular walls, obstruction to the ventricular outflow tract, and combined with the Doppler system allows us to know the gradient in the ventricular outflow tract, as a consequence of dynamic obstruction.
Gamma camera studies Radiocardiogram : preserved systolic function with increased thickness of the ventricular walls and decreased ventricle in size.
Angiography : hypertrophic left ventricle of reduced size, with mitral regurgitation and obstruction to the outflow tract of the ventricle, presenting a typical image of a ballerina's foot.
Through this method, the gradient can be measured exactly, although this can also be done with cardiac doppler echo.
Its initial treatment is medical, starting with the administration of beta blockers and calcium antagonists, the objective being the reduction of the heart rate, the decrease of the systolic function and the increase of the ventricular compliance.
In patients with frank NYHA functional class III-IV symptoms, despite medication with severe outflow tract gradients, surgical treatment with Miectomy and occasionally mitral valve replacement may be chosen.
The indication of pacemakers in these patients, in order to decrease the left ventricular outlet treatment gradient, has been carried out with mixed results.
Restrictive
This variety is the least frequent, and is characterized by diastolic dysfunction of the ventricle, without affectation of systolic function.
It is characterized by a moderate increase in the size and weight of the heart with the presence of endocardial plaques of fibrous tissue distributed in both ventricles, with
Areas that form extensive scars, giving the ventricles characteristics of hardness, roughness and lack of elasticity.
In amyloid, amyloid substance is found inside the ventricular cavities, which, as we know, is a substance of protein origin that forms true fibrils, determined by a folding of the protein structures of the amino acid sequence, being in some presentations of genetic origin, autosomal dominant type. in sarcoidosis, granulomas are found, located in the ventricular walls and in the septal regions. In hemochromatosis, true iron deposits are observed, in endomyocardiofibrosis, penetration of collagen tissue and the presence of significant interstitial edema are observed.
Symptoms : heart failure syndrome predominant as a symptom, dyspnea.
Physical examination : gallop rhythm tachycardia with R3 and R4 with occasional presence of murmurs of atrioventricular valve failure, with the rest of the semiological signs that accompany heart failure; rales, edema, hepatosplenomegaly, ascites that will appear according to the evolution of the process and the degree of involvement.
Radiology : moderate cardiac enlargement with signs of venocapillary hypertension and presence of pleural effusions.
ECG : low voltage complexes, atrioventricular and intraventricular conduction disorders.
Echocardiogram : increased thickness of the left ventricle and the mallet, with images of different intraventricular density, with preserved systolic function, and severe alteration of diastolic function.
Angiography : alteration of ventricular filling with dipplateau-type intraventricular pressure recording determined by the marked increase in intraventricular pressure, with restriction of filling.
The treatment of this type of cardiomyopathy is related to the predominant condition, heart failure or restriction of filling.
The determining etiologies have little specific treatment in sarcoidosis, arrhythmias are highly refractory to treatment, and implantation of pacemakers or cardioverter-defibrillators is indicated. Corticosteroids have been administered together with some benefits.
In the eosinophilic variant, corticosteroids together with diuretics, inhibitors of the renin angiotensin system, as in endomyocardial fibrosis.
Endomyocardial biopsy : consists of taking a sample of the heart tissue. Its indication is not general for all types of cardiomyopathies, it is related to etiological variants that are difficult to diagnose, to evaluate certain treatments or detect early rejections in transplant patients.
It consists of taking pictures of cardiac muscle under image intensifier, with a special catheter (Biotomo), in the hands of trained professionals, providing important and fundamental information for its treatment.
MYOCARDITIS
|
We call myocarditis, when the heart is undergoing an acute inflammatory process, with affectation of the heart muscle, generally caused by infectious agents.
As we can see in Table I, the etiological causes are very diverse and in many cases the clinical presentations present specific characteristics, in many of them the acute presentation can be florid in terms of specific symptoms and signs, and in other etiologies and conditions its presentation is very latent and can pass inadvertently, later evolving chronically into dilated cardiomyopathy. Variations are not only related to the etiological agent, the previous general condition of the patient is of fundamental importance.
Microscopically the cardiac size is increased, with an increase in its weight, dilated and hypertrophied.
Microscopically, an inflammatory infiltrate is observed, generally lymphocytes, degeneration of myocytes, and areas of necrosis.
Physiopathologically, when the affectation is severe, it presents the typical symptoms of heart failure, with low minute volume, it is a dilated diseased heart with impaired systolic function and frank deterioration of the ejection fraction.
Symptoms and signs . These do not differ from those that occur in heart failure syndrome, the differences are sometimes given by individualities of the pathogen or by the degree of commitment to the condition according to the previous state of the individual. The patient may present frank signs of infection, fever, restlessness, progressive dyspnea in the last days, orthopnea, and nocturia.
In the physical examination, the data can be highly variable, in some cases there is a history of having uncharacteristic "flu" symptoms, until the patient is asymptomatic and has special signs of acute involvement such as Chagas disease. In this etiology we can find the Romaña sign, bipalpebral monoocular edema with conjunctival injection and dacryoadenitis (swelling of the lacrimal gland) with satellite adenopathy of the preauricular and lateral ganglia of the neck that disappears within 30 to 40 days. Inoculation chagoma is a non-suppurative inflammatory reaction that is accompanied by a lymph node reaction and disappears after 60 days. All these processes can develop as detailed and be associated with a breakdown of the general state accompanied by fever, sweating, hepatosplenomegaly, even neurological involvement and symptoms of heart failure. Necrotic panmyocarditis with death of the patient have been observed.
In others, this acute phase does not appear and they evolve directly to the chronic stage.
Tachycardia prevails in auscultatory findings, and this in relation to the febrile picture, the presence of a 3R and 4R gallop rhythm occurs in the most severe cases, as well as the presence of an apical systolic murmur. The possibility of developing pulmonary or systemic embolisms is present.
ECG : the most frequent alterations are related to nonspecific changes in the ST segment and T wave, on other occasions atrial and ventricular arrhythmias and atrioventricular conduction disorders occur, the different degrees of AV block indisputably speak of a greater degree of involvement due to the acute process. In acute chagas, damage to the right branch of the Has de Hiss and compromise of the left anterior division are frequent, both in the acute and chronic phases.
Radiology : the cardiac size can range from normal size to severe cardiomegaly with signs of pulmonary congestion.
Echocardiogram : allows evaluating the different degrees of systolic and diastolic ventricular dysfunction, presence of thrombi, global and segmental ventricular kinesia. As it is a quick and easy method to perform without prior preparation of the patient, it allows us to periodically evaluate the patient.
Gamma camera: the administration of Gallium-67, or Pyrophosphate identifies inflammatory or necrotic changes characteristic of myocarditis.
Endomyocardial biopsy : it is very useful in some cases for the confirmation of the diagnosis, denoting that the negativity or presence of a negative biopsy does not exclude the diagnosis, which in principle is always clinical. Its repetition after a few days may be indicated.
Laboratory : high erythrosedimentation values, accompanied by leukocytosis, with neutrophilia indicate the possibilities of infectious processes. Development of different agents in blood cultures, mycological, parasitological and reactive tests for different determining agents, can enable us to approach the etiological diagnosis.
We consider that Chagas disease being an endemic in large areas of our country and that the observation of patients with this disease are very common, we must expand in more detail to provide information, in its study and diagnosis.
Diagnostic tests for chagas :
In acute stage : Microhematocrit, fresh drop: allows a rapid visualization of the agent in patients with high parasitaemia, its sensitivity is variable depending on the observer.
Indirect : Xenodiagnostic (Xd) and blood culture (Hc), for indeterminate stages (without symptoms or signs during the primary infection) and chronic with highly variable sensitivity.
Serological : direct hemagglutination, immunoflorescence, Elisa. With greater sensitivity than the previous ones, for diagnosis in indeterminate and chronic stages and for treatment evaluation.
New techniques : polymerase chain (PCR) lytic antibodies, and flow cytometry are being used.