HEAD
Skull . Inspection and palpation assess contour, regularity, and sensitivity.
The temporal arteries should be palpated and auscultated.
In newborns, the bones of the skull are separated from each other by fibrous tissue, constituting the so-called sutures. The areas where the sutures meet are called fontanelles ”(Figure 6-1). The sutures are palpable as rings and the fontanelles as depressed edges. The examination of the fontanelles should be carried out with the child calm and without effort. Sometimes the bones of the skull can be found riding one on top of the other, a fact that is produced by the passage through the birth canal and that disappears with the days.
Facies . The study of the facies allows not only to recognize the degree of health or illness of the patient, but also the state of mind and intelligence.
It is important in the inspection of the facies that there are no cosmetic fixes; According to crime novel author Agatha Christie, the truth lies beneath the makeup.
Expression, color and shape are observed.
The expression is related to muscle tone and skin coloring. There are variations within normality, being able to observe fear, anxiety, concentration, etc.
The color of the facies depends on the hematic and melanic pigments, the circulatory state of the skin and the amount of collagen tissue. These factors can vary according to race, age, sun exposure, work activity, emotion, etc.
The shape of the facies depends on the bone structure and soft tissues, which are closely related to race, age, family variations, sex, etc. Very young children may have facial asymmetry after constant supine sleep on one side, which disappears as the baby becomes more active.
Percussion of the parietal bone with the middle finger of the hand produces a broken vessel noise. Direct percussion below the zygomatic bone causes the facial muscles to contract (Chvostek's sign). This sign can persist into childhood.
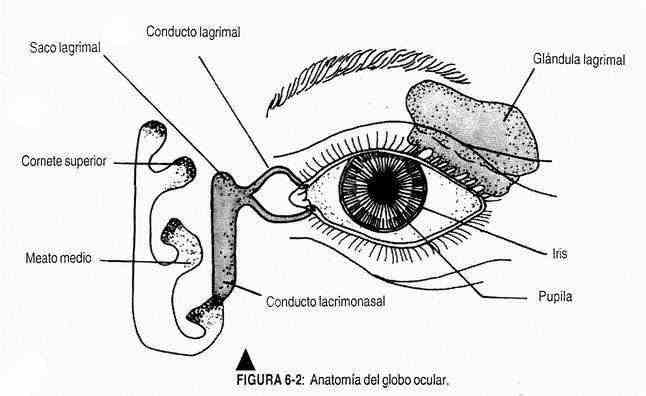
Eyes . Examination of the eyes is carried out by inspection, palpation and auscultation, and using the ophthalmoscope, flashlight, slit lamp, etc. (figure 6-2).
The eye exam begins with inspection of the eyebrows, location, and presence of hair.
Subsequently, the eyelids are observed in terms of their shape, symmetry and the presence of eyelashes. Once the inspection has been carried out, the patient's left lower eyelid is lowered with the thumb of the right hand to observe the bulbar and palpebral conjunctiva.
The same maneuver is performed with the left thumb going down to the lower right eyelid.
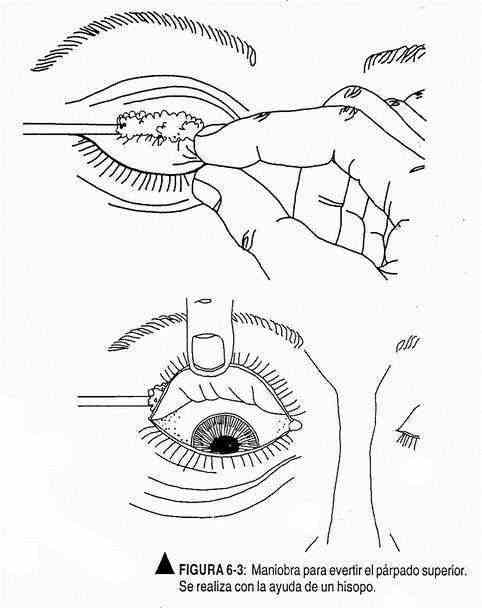
To study the conjunctiva of the upper eyelid, it must be everted (Figure 6-3). For this purpose, and while the patient looks down, the lower edge of the upper eyelid is grasped with the right index finger and thumb and, with the help of a swab, it is drawn upwards.
The conjunctiva and cornea are lubricated by the lacrimal glands; Tears drain through the tear duct, whose hole can be seen at the inner end of the upper edge of the lower eyelid. The lacrimal sac should be palpated and evaluated for regurgitation of any material into the eye.
The color of the iris is variable and depends on genetic factors. The cornea must be transparent, bright and clear when illuminated with the flashlight; its size (10 mm) and its curvature must be observed. The sclera is white.
The vascularity of the conjunctiva varies with the complexion of the individual. The robust patient will have more vascularized conjunctiva. Under normal conditions it is possible to find a small amount of discharge on the inner part of the lid margin.
The pupils must be transparent; their size, location and symmetry will be noted. The eyeballs are parallel in distance vision; the corneas, therefore, must be located in a symmetrical position.
After inspection and palpation, in some cases the eyeballs are auscultated to rule out the presence of murmurs.
The remainder of the eyeball examination is described in conjunction with the neurological examination.
Ear . It is examined by inspection, palpation, and with special procedures. It begins with the examination of the pinna or ear, whose shape and size vary according to genetic and racial factors. Usually the ear is inserted at an angle of 30 ° above the head. Their auditory function does not appear to be more important than holding glasses or wearing earrings. It is made up of the helix, antehelix, tragus, and lobe (Figure 6-4).
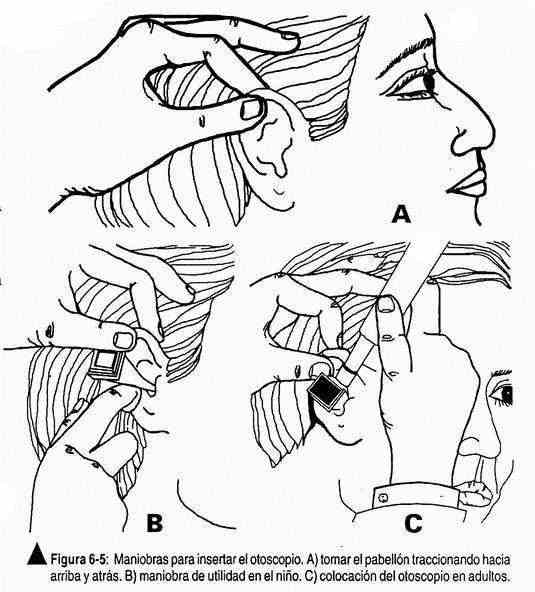
The external auditory canal is examined by rectifying the normal direction of the canal by pulling the pinna up and back.
Palpation of the preauricular area is carried out with the index finger, which leans forward, to palpate the condyle of the temporomandibular joint, which should not cause pain. Subsequently, the mastoid region is palpated, which under normal conditions should be painless.
In the external third of the ear canal there are hair follicles, sebaceous glands and earwax. At the junction of the middle and outer thirds the duct narrows to form the area called the isthmus.
The tympanic membrane, which is at the end of the canal and marks the limits of the middle ear, is seen with the aid of the otoscope. To do this, the patient rotates his head to the opposite side, the pinna is pulled up, back, and slightly out, and the otoscope is inserted (Figure 6-5).
The eardrum is an oblique membrane, sunken in its center by the malleolus, the short process of which protrudes above the hammer.
Characteristically it produces, with illumination, a reflection known as a cone of light. Its normal color is pearl gray and the anatomical parts should be located (Figure 6-6).
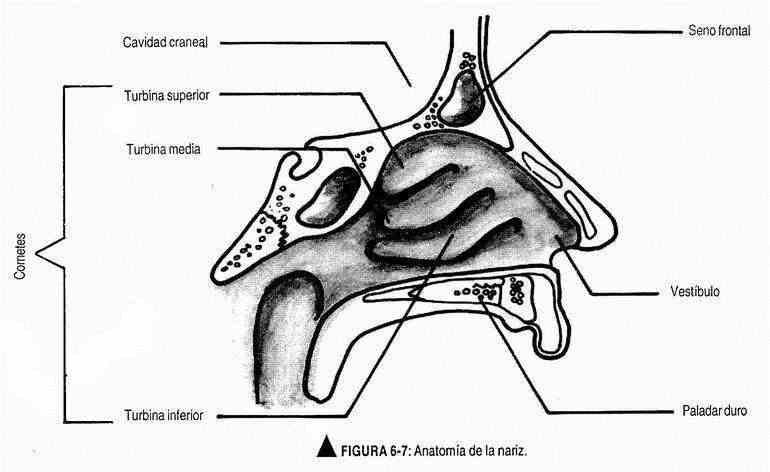
Nose . Its examination includes inspection of the nose, palpation and percussion of the paranasal sinuses, transillumination of these, and special tests such as rhinoscopy using the nasal speculum and the appropriate otoscope with a wide speculum.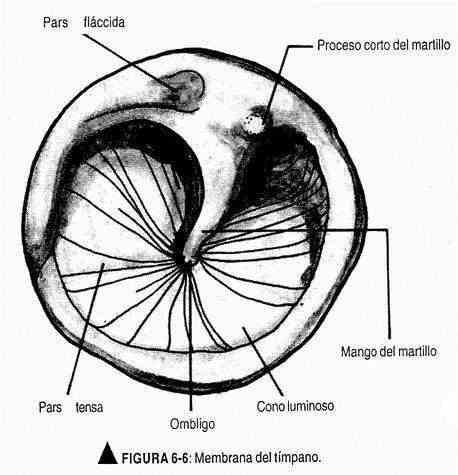
In the routine examination, the anatomical characteristics of the nose, its shape, size, coloration and symmetry are observed. The speculum is inserted with the left hand into the nostril, fixing its position with the index finger, which rests on the observed nostril. Both nostrils are observed with the same hand. The light source can be the front mirror, a flashlight or a lamp with directed light. The more practical otoscope is used with a short, wide speculum in its lumen.
The upper and lower portions of the nostrils should be examined, noting: 1) the mucosa (color and brightness), 2) the nasal septum, and 3) the middle and lower turbinates and the middle meatus (Figure 6-7).
The palpation of the frontal sinuses is carried out pressing at the level of the internal zone of the supraorbital areas, and that of the maxillary sinuses doing the same in the infraorbitrary zone, on the maxilla.
Transillumination is performed when a pathology is suspected. In a dark environment, a powerful light source is placed inside the mouth when the maxillary sinuses are to be viewed, and in the supraorbital arch when the objective is to examine the frontal sinuses. Under normal conditions, a soft reddish light is observed.
Boca . The physical examination of the mouth is done by inspection and palpation, along with special maneuvers that include the use of a rear-view mirror, a tongue depressor, and a flashlight.
The patient, sitting comfortably with his arms crossed on the lap, and the doctor, in a sitting or standing position, with the necessary elements for the examination, gets to observe the back of the tongue, the pharynx and the glottis. Percussion, such as percussion of the teeth for pain, can sometimes be helpful.
The examination of the lips consists of evaluating their shape, symmetry and mobility. The shape varies according to family and racial characteristics. An intense pink color is normal, subject to variations, and it is also possible to observe the presence of vertical lines. The patient is asked to open his mouth, and to remove any prostheses that may make the examination difficult (Figure 6-8).
Moisture is also evaluated on the lips. When opening the mouth, with the tongue blade or the fingers of the examiner and with the help of a flashlight, the inner faces of the lips and cheeks are observed, together with the gums. On the inner face of the cheeks, it is possible to find, in the jugal mucosa, a horizontal white line that represents the line of occlusion of the teeth. Also in this area are yellowish-white macules, known as Fordyce spots, which represent sebaceous glands. Stensen's orifice or parotid exit orifice is found in the jugal mucosa at the level of the second molar. The jugal mucosa is moist and pink in color, and may be pigmented with melanin in dark-skinned subjects.
At this time the gums will be examined, which must cover the alveolar process; they are pink in color and project into the interdental spaces as interdental papillae.
The teeth should be examined for their number and shape by lightly percussion with the tongue depressor or mirror, which should be painless. Mandibular occlusion will also be noted; the mouth opening should be similar in width to the width of three fingers of the patient.
The patient is then asked to raise the tongue to look at Wharton's duct (Figure 6-9), or the outlet duct of the submaxillary glands. Under normal conditions, a certain amount of saliva is found. You are then asked to open your mouth wider to examine the bony and soft palate, tonsils, and pharynx. In the bony palate, the shape and color will be observed, and the patient will be instructed to say "A" to verify the normal elevation of the soft palate. Tonsils are frequently absent due to surgical removal; They are located between the pillars of the pharynx and can be variable in size.
The patient is then asked to protrude the tongue, evaluating both its ventral and dorsal surfaces, observing its shape, size, symmetry and mobility. The mucosa of the dorsum of the tongue has fungiform-filiform papillae. The frenulum with the sublingual caruncles can be seen on the ventral side; the lingual venules that should not be prominent.
The tongue and floor of the mouth will be palpated to complete the examination of the oral cavity. Palpation should be thorough, gloved, and will evaluate the sublingual glands and tongue. The submaxillary glands can be palpated bimanually, and in the elderly as a normal feature, they can be enlarged. The parotids are located anterior to the ear and should not normally be palpable. With the mouth open, the tongue depressed by the tongue depressor, and good lighting, the pharynx can be seen, which may appear more polished.
Examination of the nasopharynx and laryngopharynx is not part of a routine physical exam. It is described in the chapter on Physical Examination for Neoplasms.
NECK
The neck is examined by inspection, palpation, and auscultation. The sternocleidomastoid, scalene, and trapezius muscles, the carotid artery, and the venous pulse should usually be identified, and the thyroid gland, laryngeal and tracheal cartilages, can be palpated. If possible, the patient should be seated, looking straight ahead, and will be asked to perform flexion-extension, rotation, lateral flexion, and neck circumduction movements to assess cervical mobility. Under normal conditions, and with the mouth closed, the patient should be able to touch the anterior aspect of the thorax with the chin.
The symmetry of the neck and the presence of carotid and venous beats will be observed. The venous pulse is described together with the cardiovascular semiology, while the carotid pulse has already been described with the vital signs.
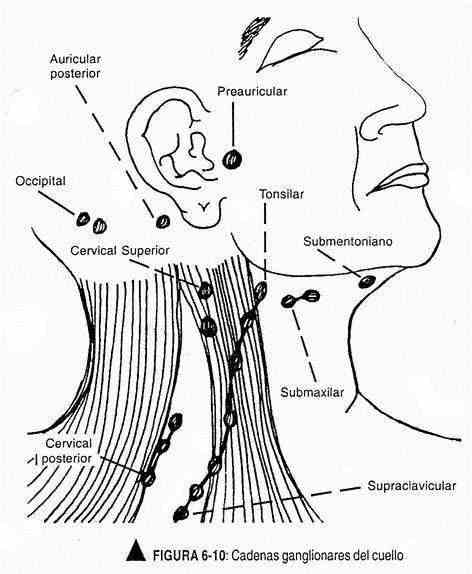
In the neck, the ganglion chains will also be palpated, where no lymphadenopathy should be found. This exam should be done in a certain order so as not to miss any node groups (Figure 6-10):
- preauricular, in front of the tragus;
- tonsillar or tonsil, in the submandibular angle;
- submaxillary, between the submandibular angle and the chin;
- occipitals; on the back of the skull;
- retroauricular, at the level of the mastoid process;
- superficial cervical, following the surface of the sternocleidomastoid muscle, and deep below it;
- anterior cervical chain, on the anterior border of the trapezius; and
- supraclavicular, between the sternocleidomastoid and the clavicle.
The trachea and the thyroid and cricoid cartilages should be identified, verifying that they are in the midline. Subsequently, the thyroid gland will be palpated, in which the shape, size, symmetry, limits, surface, consistency, sensitivity and mobility with swallowing will be described; It is advisable to give the patient a glass of water and swallow to assess mobility. Often and under normal conditions, the thyroid gland is not palpable; the isthmus can be identified as a transverse band located below the cricoid cartilage.
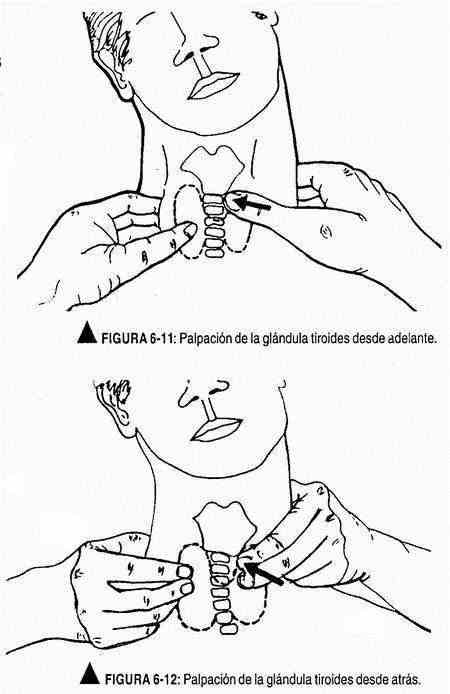
To palpate the thyroid gland, the patient will be seated, with his head slightly extended, and the examiner facing him. With the pads of both thumbs below the cricoid cartilage, the isthmus is sought, and to facilitate this maneuver, the patient is asked to swallow water or saliva. Subsequently, by flexing the head to the palpated side to flex the sternocleidomastoid muscle, the thyroid lobe is identified, while the index and middle fingers compress behind the sternocleidomastoid muscle.
The thumb of the other hand pushes the trachea toward the palpated side (Figure 6-11).
To palpate the other lobe, the same maneuvers are performed in reverse.
The thyroid gland can also be felt from behind (Figure 6-12) of the patient.
The examiner, positioned behind the patient's back, with the thumbs resting on the back of the neck, identifies the cricoid cartilage with the balls of the index and greater fingers and the thyroid isthmus below it.
The patient is asked to swallow and the fingers are moved slightly to the sides to feel the lobes, again asking him to swallow. Then the neck is flexed slightly forward and to the right, displacing the right thyroid cartilage with the fingers of the left hand, palpating with the right hand, the thumb is placed deeply and behind the sternocleidomastoid and the index and middle fingers in front of him. The patient is asked to swallow. To palpate the opposite side, the reverse procedure is carried out.
The thyroid gland should be auscultated to verify the absence of murmurs. Also, and with the same objective, the carotid arteries should be auscultated.